Telemedicine – Just What the Doctor Ordered
By Brian Wallace
January 10, 2024 • Fact checked by Dumb Little Man
Telemedicine has become vital in all areas of healthcare in the past year. Since the onset of the pandemic, telemedicine has been a very common way of conducting visits and continuing patient care across the board. Still, one of the communities hit the hardest by the COVID pandemic is nursing home residents and their staff.
Nursing home residents are some of our most vulnerable population, but sadly, it has been made 100% clear that these facilities need to be updated and experience an operations overhaul as they were terribly ill-equipped to manage the unforeseen demands of a global pandemic. This is why nursing homes must be included in the progress of telemedicine in order to survive and thrive.
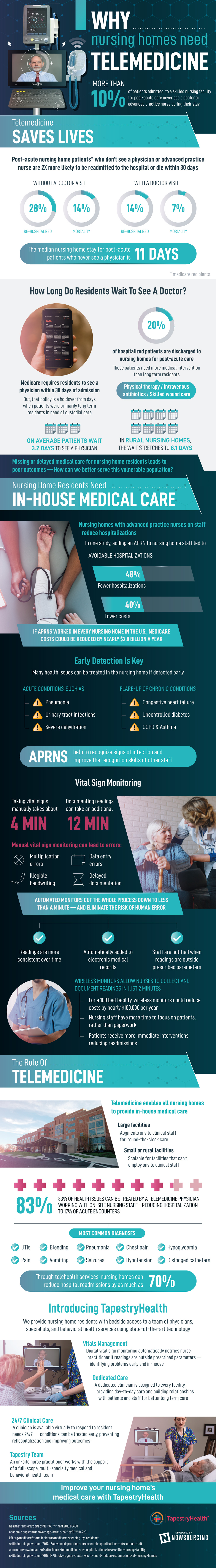
Telemedicine can save lives in nursing homes
Currently, 10% of post-acute patients who are admitted to nursing homes, never see a physician for follow-up. Sadly, this means that their re-hospitalization and mortality rates double compared to those who receive follow-up care. Within the first 30 days, 28% of post-acute patients, who do not see a doctor, will be re-hospitalized, and 14% of them will die. However, if these same patients have access to a doctor then only 14% will be re-hospitalized, and 7% will die in that same time period. The median stay for post-acute patients who never see a doctor is just 11 days.
Twenty percent of all hospitalized patients are discharged to nursing homes for post-acute care, and these patients require more medical attention in the nursing facility in order to be able to heal and thrive. They need things like physical therapy, intravenous antibiotics, and wound care. Medicare does require that patients see a physician within 30 days of admission, but this protocol is outdated as it was implemented when patients were primarily there for the long haul and only needed custodial care.
Currently, the average wait for a patient to see a physician is 3.2 days for urban areas, but in rural areas, this increases to an average of 8.1 days. So, the issue is that patients are either not seeing physicians at all, or they are having to wait too long to see them, which naturally leads to poor medical outcomes.
⫸ Nursing home residents must have in-house medical care in order to be served well.
Statistically, nursing homes that employ advanced practice nurses (APRN) reduce hospitalizations. One study shows that the presence of an on-site APRN can reduce hospitalizations by up to 48%. This also means lower overall costs at a reduction of 40%. If an APRN was on-site in every nursing facility in the US, Medicare costs could be reduced by nearly 2.8 billion dollars per year.
⫸ Early detection of medical issues is a huge factor in these hospitalization and cost reductions.
Of course, this is something that an APRN will be able to do with more skill than lesser trained nursing staff. If detected early, many common health issues can be treated in the facility. Acute conditions, such as pneumonia, UTIs, and severe dehydration, as well as flare-ups of chronic conditions, such as congestive heart failure, uncontrolled diabetes, COPD, and Asthma, can all be treated in the nursing facility. APRNs will be able to recognize early signs of infection and to improve the recognition skills of other staff members as well.
⫸ Vital signs monitoring is another area where care could be improved and costs of both time and money can be reduced.
It takes about 4 minutes to take vital signs manually, and an additional 12 minutes to document the readings. Manual monitors can also lead to mistakes such as multiplication errors, data entry errors, illegible handwriting, and delayed documentation.
Implementing automated monitors cuts the entire process down to one minute, and removes the “human error” factor completely. This means that readings are more consistent over time, they’re automatically added to patient’s records, and staff is notified of any concerns.
Wireless monitors also allow nurses to collect and document readings in just 2 minutes. This could reduce costs by about 100,000 dollars per year for a 100-bed facility. This also means that nursing staff can spend more time focusing on patients and patients will receive more immediate care.
Beyond all of this, telemedicine is key to improving all medical care provided in nursing homes by enabling every nursing home to have access to physicians. Large facilities can use telemedicine to augment nursing staff to provide round-the-clock care. Telemedicine is also scalable so that small or rural, that can’t employ on-site clinical staff, can still have access to physicians and APRNs whenever they need them.
Coordination and cooperation between telemedicine physicians and on-site nursing staff mean that 83% of medical conditions can be treated in-house and hospitalizations due to acute encounters can be reduced to just 17%. The most common diagnoses, such as UTIs, bleeding, pneumonia, chest pain, hypotension, seizures, and hypoglycemia, can all be treated in-house. Nursing homes can also reduce hospital readmissions by 70% when working in conjunction with telemedicine physicians.
After what nursing home residents and their families experienced last year, it’s clear that nursing homes need additional help to ensure the necessary care for their patients. By employing on-site APRNs, implementing the use of automated and wireless monitors, and introducing telemedicine to daily operations, nursing homes can become the best place for post-acute patients and long-term residents to receive exactly the kind of care that they need and deserve.
Brian Wallace
Brian Wallace is the Founder and President of NowSourcing, an industry leading infographic design agency based in Louisville, KY and Cincinnati, OH which works with companies that range from startups to Fortune 500s. Brian also runs #LinkedInLocal events nationwide, and hosts the Next Action Podcast. Brian has been named a Google Small Business Advisor for 2016-present and joined the SXSW Advisory Board in 2019.